The Board of Nursing (BON) exists to promote, preserve and protect the safety, welfare and public health of the entire public through registered professional education, control of practice and practical nursing and legislative regulation.
Contents:
- The GA Board of Nursing Services
- Board of Registered Nursing
- General Practice Information
- Advanced Practice Information
- Nursing Practice Act
- The GA Board of Nursing Licensing
- The GA Board of Nursing Education Program Approval
- The GA Board of Nursing Enforcement
- The GA Board of Nursing Continuing Education Requirements
- The GA Board of Nursing Endorsement
The GA Board of Nursing Services

The GA Board of Nursing carries out this statutory mission by providing services in various areas including:
- Licensing
- Nursing Education Program Approval
- Enforcement
- Information
Board of Registered Nursing

Board of Registered Nursing (BRN) advocates and protects the safety and health of the entire public by ensuring the best quality registered nurses (RNs) in various states. Some state boards of nursing approved by the BRN include:
- Georgia Board of Nursing
- California Board of Nursing
- Virginia Board of Nursing
- Oklahoma Board of Nursing
- Kentucky Board of Nursing
- Arizona State Board of Nursing
- Louisiana State Board of Nursing
- Arizona Board of Nursing
- Nevada State Board of Nursing and others
General Practice Information
BRN provides the general practice information such as nursing practice information, guidelines, and advisories to guarantee ongoing communication of proficiency standards for registered nurses, consumers, educators, employers, and other regulators. This information is often updated due to the changes and growth of the scope of Registered Nursing practice.
Advanced Practice Information

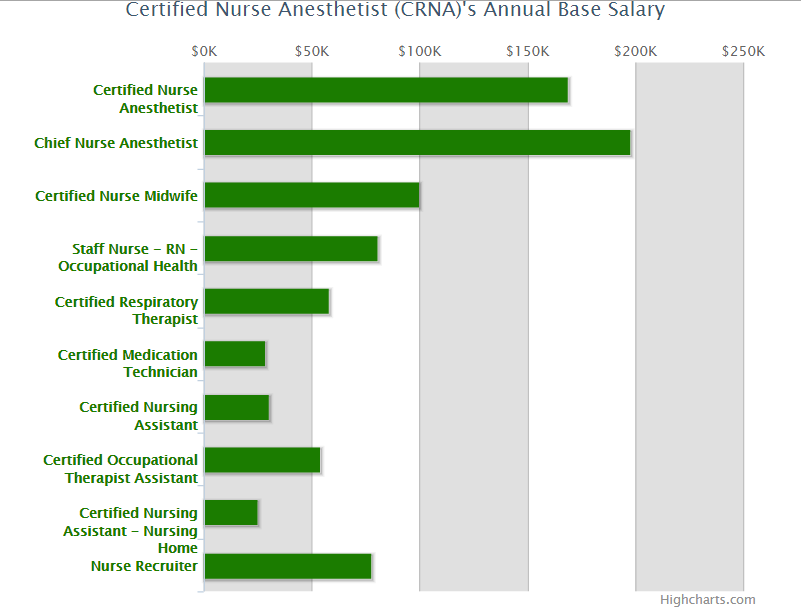
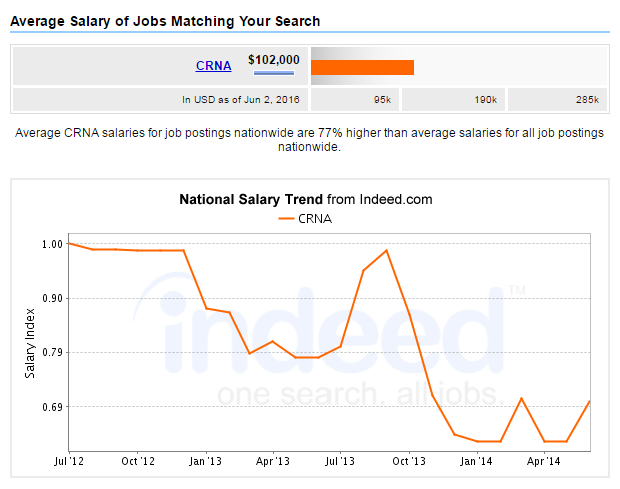
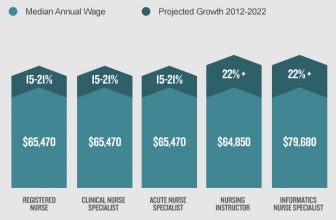
BRN also provides advanced practice information, guidelines, and advisories to guarantee ongoing communication of proficiency standards to employers, consumers, educators, regulators and advanced practice nurses, including nurse midwives, nurse practitioners, nurse anesthetists, clinical nurse specialists, and psychiatric or mental health nurses). Numerous updates in information are due to the changes and development/growth in the scope of Advanced Practice Nursing.
Nursing Practice Act
The nursing practice act (NPA) is the body of state laws that mandate the boards of nursing to outline the responsibilities and scope of practice for registered nurses. Nurses are required to comply with or follow the law & related rules to maintain their nursing licenses. The nursing practice act describes:
- Qualifications for licensure
- Nursing titles which are allowed or recommended to be used
- Scope of practice, nurse specialty or what RN is allowed to practice
- Actions that might or will happen in case the nurse doesn’t follow the nursing laws, rules or regulations
The GA Board of Nursing Licensing
The GA Board of Nursing offers licenses for nurses through examination & endorsement from other recognized states. The board also approves qualified Registered Nurses (RNs) to enter practice as Advanced Practice Nurses (APRNs), including nurse practitioners, nurse midwives, clinical nurse specialists, and nurse anesthetists.
License applications are regularly reviewed within 15 business days from issuance of receipt of every required document. Issues like previous disciplinary actions or past criminal behavior may prolong these time duration specifically to allow for disciplinary or board staff review.
Licensure services include:
- Approval of the applicant before sitting for the NCLEX
- Issuance of a license after successful examination
- Issuance of permanent license upon completing all application requirements
- Renewal of the nursing license
- Approval of full APRN’s authorization upon completing all application requirements
- Renewal of an APRN authorization
The GA Board of Nursing Education Program Approval

The GA board of nursing approves all nursing education programs which effectively prepare nurses for first entry into the nursing practice. Currently, there are 25 practical nursing education programs and 51 registered nursing education programs approved by the Georgia board of nursing.
Nursing education program approval services include:
- Annual review of the approval status of every nursing education program
- Routine site visits of every nursing education program to decide continuing education approval status. Additional site visits might be scheduled while responding to complaints from consumers or a drop in the pass rate of graduates who sit the NCLEX
- Guidance and consultation for programs that do not comply with the Board’s regulations
The GA Board of Nursing Enforcement

The GA board of nursing enforces the Board Rules & Regulations and Nursing Practice Act (NPA) by deciding minimum standards to support nursing education and nursing practice, adjust complaints, and conduct investigations of various complaints against nurses.
To administer enforcement, the board is approved to take any of these disciplinary actions:
- Refuse to renew or grant a license to the applicant
- Administer a private or public reprimand
- Suspend any nursing license for a definite/indefinite period with all conditions that can be attached to restoring the said license
- Restrict or limit any license when the board considers necessary for public protection
- Revoke any license
- Withhold pending formal disposition or condition a penalty upon the licensee’s or applicant’s submission to such counseling, treatment, or care as per the board’s directive
- Impose a fine for each violation of the law, rule or regulation related to the nursing practice
- Impose on an applicant or licensee charges or fee in an amount fundamental to reimburse the board for the legal and administrative costs incurred by the board in disciplinary proceedings or conducting an investigative
Any person who knows of any conduct or practice by a licensed nurse that violates the Board Rule, GA Nurse Practice Act, or related federal or state law can report the alleged violations to the Georgia board of nursing.
The GA Board of Nursing Continuing Education Requirements

The Georgia board of nursing has continuing education requirements for practical nurses as well as registered nurses.
Practical Nurses
All licensed practical/practice nurses must complete 20 hours of continuing education for license/licensure renewal. Practice nurses can also meet licensure renewal requirements by completing an accredited or approved academic program/course in registered professional nursing, as certified by the board.
If audited, the applicant or licensee must submit all documentation upon completing one of the 2 options.
Registered Nurses
All registered nurses must complete the competency requirements or continuing education for license/licensure renewal. Registered nurses can also meet licensure renewal requirements through the following options:
- Completion of 30 hours of continuing education by a board approved provider
- Maintenance of re-certification or certification by a national certifying body identified by the board
- Completion of an approved/accredited academic program in nursing or any other related fields as identified by the board
- Verification of competency or proficiency by an entity, physician’s office or health care facility, and at least 500 hours of practice as shown by your employer
- Completion of a board certified/approved graduation or re-entry program from a program of nursing education
If audited, the applicant or licensee must submit all documentation upon completing one of the 5 options. Licensees or applicants are selected for renewal audit, once they submit the renewal application.
If licensees or applicants don’t complete or meet the audit requirements, their licenses aren’t renewed due to submitting an incomplete renewal.
Please note, GA Board of Nursing doesn’t approve individual CE providers.
The GA Board of Nursing Endorsement

The GA board of nursing offers licensure through endorsement if the licensees meet the requirements below:
- Individuals who are licensed as a registered nurse (RN) in another state must provide evidence of at least two years of Clinical Nursing Practice within the past three years in order to apply for licensure through endorsement. A $60 application fee is also required.
- Individuals who are licensed as a practical nurse in another state must provide proof of at least two years of Clinical Nursing Practice within the last three years in order to apply for licensure through endorsement. A $75 application fee is also required.
Overall, licensees are required to renew their licenses every two years. To renew your nursing license, please visit the GA Board of Nursing website. It is very essential to maintain all contact information for your state’s board of nursing, this is to ensure that you stay updated about all state laws, rules & regulations regarding continuing education, licensing renewals, fees and charges, and much more. Make sure you contact the GA board of nursing to update your practice and contact information and renew any licensing.
SOURCES: